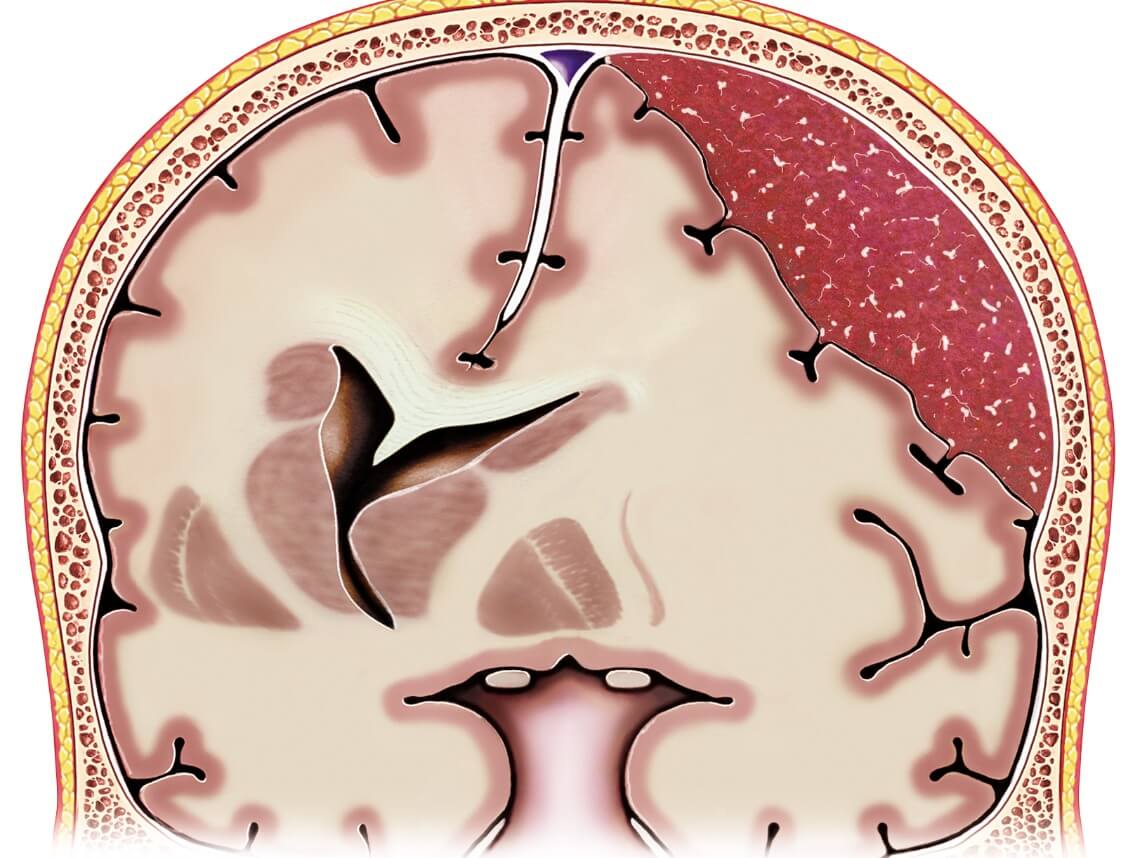
Subdural hematoma in children is characterized by the accumulation of blood between the brain and the dura mater, the tough outer covering of the brain. It usually occurs as a result of head trauma or injury. Here’s a breakdown of the symptoms, causes, diagnosis, treatment, recovery, and care associated with subdural hematoma in children:
Subdural Hematoma Symptoms
- Headache
- Vomiting
- Changes in behavior or personality
- Seizures
- Drowsiness or lethargy
- Irritability or fussiness
- Loss of consciousness
- Poor appetite
- Weakness or difficulty walking
- Developmental regression (in infants)
Subdural Hematoma Causes
The most common cause of subdural hematoma in children is head trauma, such as falls, car accidents, or physical abuse. The condition can occur in infants due to non-accidental trauma (shaken baby syndrome) or during childbirth if there is significant head compression.
How is subdural hematoma diagnosed?
Diagnosing a subdural hematoma typically involves a combination of medical history evaluation, physical examination, and imaging tests. The doctor may order a computed tomography (CT) scan or magnetic resonance imaging (MRI) to visualize the brain and detect the presence of bleeding.
Treatment of Subdural Hematoma in Children
Treatment options depend on the severity of the subdural hematoma. Mild cases may be managed conservatively with close observation, while more severe cases often require surgical intervention. Surgical treatment involves draining the accumulated blood and relieving pressure on the brain. The specific surgical procedure may vary based on the child’s age, the size of the hematoma, and the child’s overall condition.
Subdural Hematoma Recovery
Recovery from a subdural hematoma can vary depending on the severity of the condition and the promptness of treatment. Some children may recover fully with minimal long-term effects, while others may experience neurological deficits or developmental delays. The recovery period can span several weeks to months, often involving close monitoring, rehabilitation, and follow-up appointments with healthcare professionals.
Caring for a Child with Subdural Hematoma
During the recovery process, providing proper care and support is crucial. Here are some essential aspects of care:
- Medication: Follow the prescribed medication regimen, including pain relief and any other medications the healthcare provider recommends.
- Rest: Ensure the child gets plenty of rest and avoids strenuous activities to allow the brain to heal.
- Observation: Watch for any changes in behavior, symptoms, or complications and promptly report them to your healthcare provider.
- Nutrition: Provide a balanced diet to promote healing and overall well-being.
- Rehabilitation: If necessary, engage in rehabilitative therapies, such as physical therapy, occupational therapy, or speech therapy, to aid in recovery and regain lost abilities.
- Emotional support: Offer emotional support to the child and family members, as recovering from a subdural hematoma can be a challenging experience emotionally.
It is essential to consult a healthcare professional for a comprehensive evaluation, accurate diagnosis, and appropriate treatment plan for a subdural hematoma.
Contact Care Options for Kids for Home Health Care in Florida
It can be hard to balance your time between work, home, and caring for a child. That’s why our team of skilled professionals at Care Options for Kids is here to help.
Our home health care services offer one-on-one care in the comfort of your home. We refer loving and competent nurses to provide customized care for families — from a few hours a day to around-the-clock supervision. Contact us directly to speak with a home health care professional or request a free Pediatric Consultation. Together we can determine the best plan of action to keep your loved ones happy and healthy.
If you or a loved one are considering Pediatric Home Health Care Services in Florida, contact the caring staff at Care Options for Kids. Call today at (888) 592-5855.