We’ve all known a child who turns their nose up at broccoli or insists their spaghetti shouldn’t touch their meatballs. But for some children, the challenges around eating go far beyond picky preferences. These challenges can include gagging when trying new foods, severe aversions to certain textures or smells, difficulty chewing or swallowing, and even complete refusal to eat.
Mealtimes, instead of being moments of connection, can become scenes of anxiety, tears, and frustration — for both the child and their caregivers. For children struggling with feeding challenges, eating, drinking, and swallowing may not just be difficult — they can be physically painful and emotionally frightening. Over time, these issues can impact not just nutritional health, but also a child’s physical growth, cognitive development, and social and emotional well-being.
Fortunately, with early intervention and support through pediatric feeding therapy, families can find practical solutions that help children become happy, healthy eaters.
What Is Pediatric Feeding Disorder?
Pediatric Feeding Disorder (PFD) is generally defined as any non-age-appropriate impaired oral intake. Children with PFD may eat very little, avoid entire food groups, struggle to chew or swallow safely, or experience physical discomfort during or after meals.
This goes far beyond normal mealtime pickiness and requires specialized care and attention.
There are an estimated one in 37 children under the age of five in the U.S. are affected by PFD each year. Even more telling, research shows that up to 25% of all children and as many as 80% of children with developmental delays are believed to have some type of feeding disorder. The consequences can be serious — leading to growth failure, compromised immune function, developmental delays, and even life-threatening complications if left untreated.
Causes of Pediatric Feeding Difficulties
The root causes of feeding disorders are often complex, including:
- Medical issues, such as gastrointestinal disorders, allergies, or respiratory conditions.
- Neurological impairments, including those caused by stroke, cerebral palsy, or traumatic brain injury, which can interfere with oral motor coordination.
- Sensory processing disorders, where a child’s nervous system struggles to process input like texture, taste, temperature, or smell, often resulting in strong aversions.
- Developmental disorders such as autism spectrum disorder (ASD) may affect a child’s relationship with food, routines, and sensory experiences.
- Behavioral or psychological challenges, including anxiety or past traumatic feeding experiences, such as prolonged NICU stays or tube feeding.
No matter the underlying cause, the experience of pediatric feeding difficulties is often overwhelming for families. Fortunately, pediatric feeding therapy offers a comprehensive, individualized path forward.
Pediatric Feeding Therapy: What It Is and How It Helps
At its core, pediatric feeding therapy is the process of teaching children how to eat — or how to eat better — in a safe, supportive, and individualized way. This therapy goes far beyond simply coaxing a child to take “one more bite.” It requires an in-depth understanding of a child’s medical, sensory, motor, and behavioral challenges.
Pediatric feeding therapy is usually provided by a multidisciplinary team that may include:
- Speech-language pathologists (SLPs) who assess swallowing function and oral motor skills
- Occupational therapists (OTs) who support sensory integration and self-feeding skills
- Dietitians or nutritionists who monitor nutritional intake and create safe, balanced meal plans
- Medical professionals, such as pediatricians, nurses, or gastroenterologists, who oversee medical care
- Developmental specialists or psychologists who address emotional, behavioral, and relational aspects of feeding
With the help of professionals, families can receive expert support from therapists trained specifically in pediatric feeding therapy. These specialists tailor every treatment plan to the individual needs of the child, supporting not only the child’s development but also helping caregivers navigate feeding with confidence and compassion.
Assessment: The First Step in Pediatric Feeding Therapy
Before any child begins pediatric feeding therapy, a thorough and multidisciplinary assessment is essential to determine if your child needs feeding therapy. Feeding challenges are rarely caused by a single issue, which is why this evaluation goes far beyond observing eating habits. Instead, it is a holistic process that helps therapists understand the child’s medical, developmental, sensory, behavioral, and nutritional needs, so they can build a treatment plan that’s both individualized and effective.
A comprehensive pediatric feeding assessment typically includes the following key components:
1. Medical History Review
Understanding your child’s medical background lays the foundation for effective therapy. Therapists, often in collaboration with medical providers, will review:
- Birth history, including premature birth, NICU stays, and delivery complications
- Past and current diagnoses, such as reflux, food allergies, and chronic respiratory illness
- Surgical history, such as gastrointestinal surgeries or tracheostomies
- Medication use and how it may affect appetite or digestion
- Growth charts and weight gain history
- Any history of feeding tubes or specialized nutritional support
This medical context helps therapists identify physiological contributors to feeding difficulties and ensures that interventions are safe and medically appropriate.
2. Feeding History and Behavior
Parents and caregivers are invaluable sources of insight. During this part of the assessment, the therapist will ask detailed questions about the child’s daily feeding routines and history, including:
- Age at which solid foods were introduced
- Bottle or breastfeeding experiences
- Length and frequency of meals
- Preferred and non-preferred foods
- Patterns of food refusal or avoidance
- Mealtime behaviors, such as tantrums, spitting, gagging
- Use of utensils or self-feeding skills
This information helps therapists determine whether a child’s feeding behaviors are age-appropriate or indicate deeper issues that need to be addressed.
3. Oral-Motor and Swallowing Evaluation
Feeding is a complex motor skill involving coordination between the lips, tongue, jaw, and throat. During this part of the assessment, therapists will examine:
- Lip closure and strength
- Tongue mobility and coordination
- Jaw stability and chewing efficiency
- Sucking and sipping skills for liquids
- Swallowing patterns and signs of dysphagia
- Coordination between breathing and swallowing
Children who exhibit signs of aspiration, when food or liquid “goes down the wrong pipe”, may be referred for an instrumental swallow study, such as a modified barium swallow study or a fiberoptic endoscopic evaluation of swallowing, to further evaluate swallowing safety.
4. Sensory and Behavioral Observation
For many children with pediatric feeding disorders, sensory processing difficulties can make mealtime a stressful experience. The therapist will observe the child’s reactions to:
- Different food textures, such as crunchy, smooth, and mixed
- Temperatures, including cold versus warm foods
- Smells and colors of foods
- Utensils, high chairs, and feeding environments
Children may display signs of distress such as crying, gagging, pushing food away, or refusing to sit at the table. These behaviors help therapists understand how sensory sensitivities might be interfering with feeding.
5. Nutritional Evaluation
Nutrition is a core aspect of the assessment and is often completed by a registered dietitian as part of the pediatric feeding therapy team. The dietitian will:
- Evaluate current intake of calories, fluids, and essential nutrients
- Compare dietary intake to age-appropriate nutritional needs
- Assess for signs of malnutrition, dehydration, or vitamin/mineral deficiencies
- Look at food variety and whether key food groups are being excluded
- Discuss any special diets, such as allergy-based, texture-modified, or tube-fed nutrition
The nutritional assessment ensures that the child’s health and growth remain top priorities throughout the therapy process.
6. Developmental Screening
Feeding skills develop alongside other milestones — like fine motor skills, communication, and cognitive abilities. As part of the assessment, therapists may conduct or request a developmental screening to evaluate:
- Gross and fine motor development, including sitting stability, pincer grasp
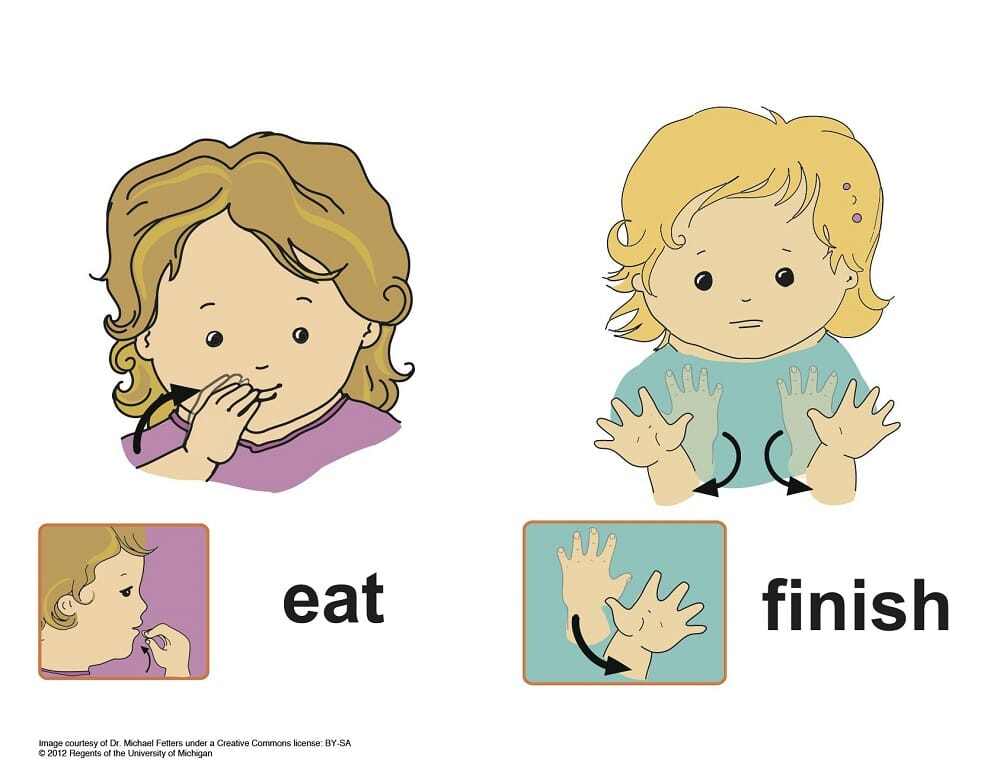
- Communication abilities, such as verbal, nonverbal, or the use of augmentative devices
- Social and emotional development
- Cognitive functioning and attention span
Children with developmental delays may need support across multiple domains, and understanding these areas helps therapists set realistic and appropriate feeding goals.
7. Family Dynamics and Feeding Environment
Feeding is not just a physical task — it’s deeply relational. The family’s approach to mealtimes, cultural practices, stress levels, and overall dynamics all influence feeding outcomes. Therapists will observe or ask about:
- Typical mealtime routines and settings, including whether the TV is on or off, or if the family is seated at a table
- Who feeds the child, and how they respond to refusals or messes
- Parent-child interactions during meals
- Emotional tone of mealtimes — are they rushed, tense, or relaxed?
- Cultural or religious food preferences or restrictions
By evaluating the environment where feeding takes place, therapists can suggest practical strategies that support both the child’s progress and the family’s unique needs.
Building the Pediatric Feeding Therapy Plan
Once the full assessment is complete, the feeding therapy team develops a customized pediatric feeding therapy plan. This plan includes:
- Specific, measurable therapy goals tailored to the child’s needs
- Recommended frequency and setting for therapy, including in-home, clinic-based, or hybrid
- Strategies to improve oral motor function, increase food variety, reduce sensory aversions, and promote positive mealtime behaviors
- Nutrition and hydration goals, when appropriate
- Caregiver education and at-home strategies to support progress
This collaborative, individualized approach is what makes pediatric feeding therapy so effective. It’s less about one-size-fits-all solutions — it’s about honoring each child’s journey and empowering families with tools for success.
The Connection Between Feeding Therapy and Swallowing Disorders
Many children receiving pediatric feeding therapy also experience swallowing disorders, known as dysphagia. Dysphagia refers to difficulty or discomfort in swallowing and can present in a variety of ways:
- Coughing or choking during meals
- Frequent respiratory infections or pneumonia
- Refusing to eat or drink
- Holding food in the mouth without swallowing
- Slow or effortful eating
For these children, feeding therapy not only targets food acceptance but also emphasizes safe swallowing strategies. Therapists may recommend specific textures, teach compensatory techniques, or introduce special feeding tools to support safer intake.
By addressing both feeding aversions and swallowing safety, pediatric feeding therapy can help children build confidence while reducing medical risks associated with dysphagia.
What to Expect During Pediatric Feeding Therapy
Every child is different, and so is every therapy session. Pediatric feeding therapy can take place in a clinic, a hospital, or even better — right in the comfort of your home. In-home therapy offers a unique opportunity for children to practice eating in familiar surroundings using their own utensils, chairs, and foods.
Common Goals and Techniques in Therapy
Depending on a child’s needs, therapy may include:
- Oral motor skill development, including jaw strengthening, lip closure, and tongue mobility.
- Swallowing exercises and techniques to reduce aspiration risks.
- Desensitization to textures or smells through gradual exposure in a safe, playful setting.
- Mealtime routine building, creating structure and predictability to reduce anxiety.
- Self-feeding skill development, including grasping utensils and bringing food to the mouth.
- Food chaining, where a child is slowly introduced to new foods through small, manageable changes from their preferred foods.
Each session is tailored with care, intention, and patience — because the ultimate goal is not just for children to eat, but to enjoy eating and all the social, cultural, and emotional connections it brings.
Supporting Your Child at Home
As a parent or caregiver, your role in pediatric feeding therapy is incredibly important. Children thrive when they feel safe, supported, and understood. Here are some tips for caregivers navigating the journey of PFD:
- Create a stress-free environment at mealtimes, and avoid pressuring or bribing your child to eat
- Establish consistent routines around meals and snacks to help children know what to expect
- Celebrate small victories — trying a new food, sitting at the table, or even smelling something new
- Communicate regularly with your therapy team and follow through with home strategies
- Practice patience and compassion, both for your child and yourself
Feeding challenges can be emotionally draining, but you’re not alone. The support of a professional pediatric feeding therapy team can help lift the burden and bring joy back to mealtime.
The Benefits of In-Home Pediatric Feeding Therapy
Choosing in-home therapy offers families an extra layer of comfort and convenience:
- Familiar surroundings: Children are more likely to feel relaxed and engage in therapy when they’re at home.
- Consistency of care: Having the same clinician regularly leads to deeper trust and more personalized progress.
- Practical application: Therapists can work directly with your kitchen setup, your food routines, and your family members — making therapy more effective and easier to implement.
Families who choose in-home services often find therapy becomes a natural part of daily life — rather than another appointment to squeeze in.
A Brighter Future With Pediatric Feeding Therapy
No parent wants to see their child struggle, especially with something as fundamental as eating. But with early diagnosis, compassionate care, and the right therapy plan, most children with PFD can make tremendous progress. Pediatric feeding therapy is a gentle, evidence-based partnership between families and professionals to help children grow, thrive, and find joy in food again.
If you suspect your child may be experiencing feeding difficulties, don’t wait. Seek help early. Pediatric feeding therapy can be life-changing — not just for your child, but for your entire family.
Care Options for Kids is here to support you every step of the way. With expert therapists who come to your home, individualized care plans, and a deep commitment to your child’s well-being, we believe that every child deserves the opportunity to eat well, grow strong, and thrive.
Let’s make mealtimes a source of connection — not conflict.
Schedule Your Child’s Care Assessment Today
At Care Options for Kids, we understand the unique challenges of caring for a child with health conditions. Our dedicated team of pediatric home health nurses is here to support your family with compassionate, expert care tailored to your child’s needs. Contact us today to schedule an assessment and learn how we can help you navigate this journey with confidence and care.
Click here to start your journey to better care.
This post is for educational and informational purposes only. You should always speak with your own therapist before implementing this information on your own.