Transitioning to telepractice as a clinician presented its own set of hurdles, reminiscent of the early days of my career with the exhaustive hours dedicated to session preparation. Despite years of experience, there are still moments that demand innovative solutions.
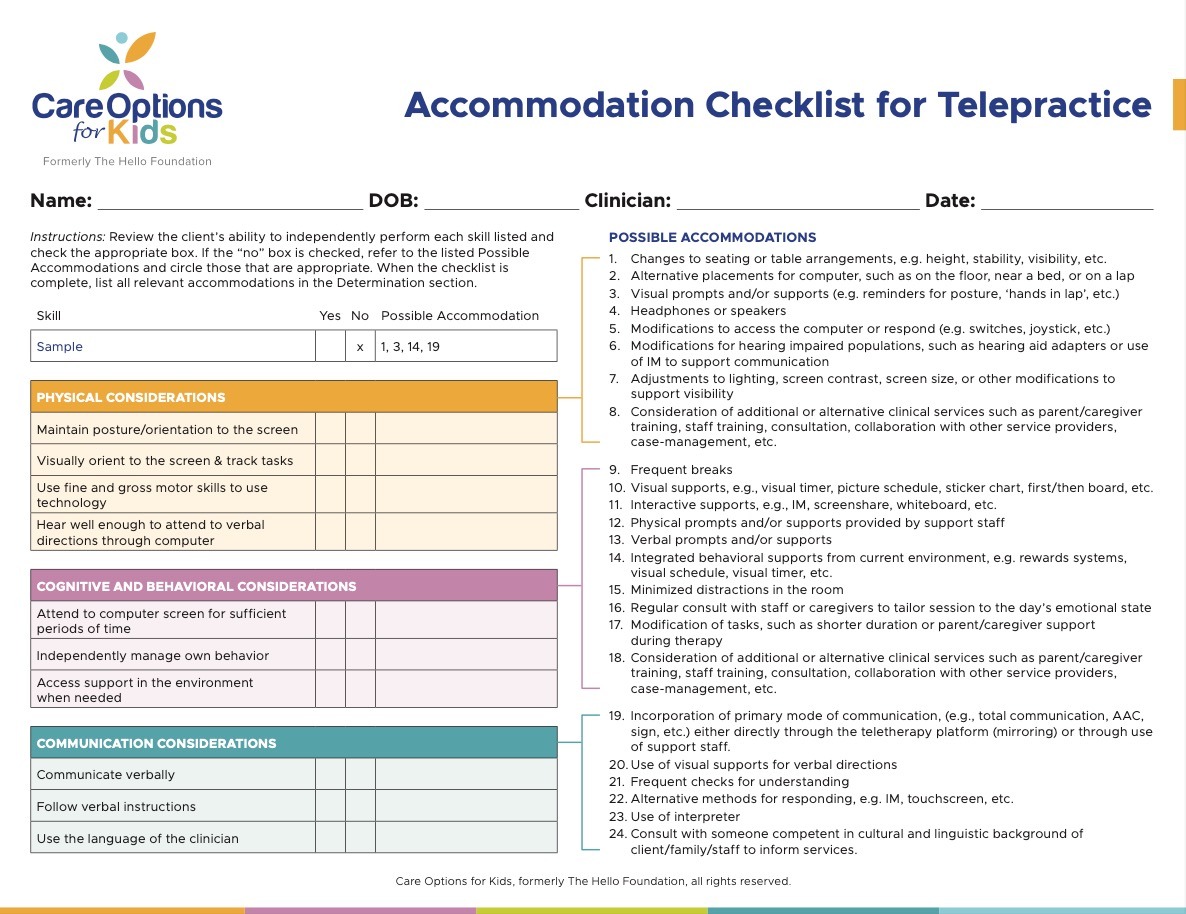
The Accommodation Checklist for Telepractice has been invaluable in guiding discussions and ensuring students receive tailored support regardless of the medium. This tool is designed to guide teams through these tough conversations. This checklist allows teams to look at Physical, Cognitive, Behavioral, and Communication considerations, and then decide what sort of accommodations need to be made to remove the barriers to accessing services via telepractice. It also has a section to guide the discussion about what sort of Support Resources the student might need, as well as an area to delegate roles and responsibilities and to decide appropriateness. Read on to learn how it works, then download it for free below!
Physical considerations and accommodations for telepractice
Physical considerations in telepractice encompass how a student interacts with the technology. This section prompts the team to assess the student’s requirements for maintaining screen orientation, tracking tasks, and executing fine and gross motor activities like typing and pointing. Additionally, it addresses auditory aspects, ensuring the student can effectively hear both the clinician and themselves during therapy. If additional support is deemed necessary, the checklist provides a range of accommodations, including adjustments to lighting or screen contrast, alternative computer placements, and utilization of assistive technologies such as switches and joysticks.
Cognitive and behavioral considerations and accommodations for telepractice
Attention and behavior support are crucial elements, especially in a remote setting. Can the student engage independently? Are distractions minimized? What about asking for help when they need it? These questions prompt tailored interventions, such as visual supports and task modifications. Possible accommodations in this area include visual supports, minimized distractions, consult with on-site staff regarding the day’s emotional state, and modification of tasks and duration of sessions.
Communication considerations and accommodations for telepractice
Students who are receiving speech-language services have special communication needs by definition. This section asks teams to dive a little more deeply, however, and consider the nature of those needs and how they specifically relate to telepractice. If the student is not yet communicating verbally, for example, it will be essential that their primary mode of communication be integrated into the sessions. Likewise, accommodations will need to be made if the student and clinician are not proficient in the same language.
Support resources considerations
This section asks a team to think about the technology itself (e.g. computer, webcam, internet connection) as well as the support personnel who are available for the purpose of telepractice.
Determination
The checklist culminates in a comprehensive plan, outlining necessary accommodations and implementation notes. This final step ensures clarity regarding roles and responsibilities and facilitates informed decision-making regarding the suitability of telepractice for the student.
We love this accommodations checklist because it takes the focus off the telepractice model. It turns the conversation toward the student’s skills and needs, and the capabilities of all the people on the team. By looking at the time, space, knowledge, and supports that are available, an IEP team can decide how to spend them in a way that is sustainable and agreeable to the whole team. It’s been used by teams serving just about every type of student you can think of — preschoolers, AAC users, students with limited vision or mobility, students with challenging behaviors — and on teams that are facing their own internal challenges as well. Give it a try with your easiest and your toughest cases, and let us know what you think!